Practice Tactics
Clarified Guidelines for Expedited Requests
Umpqua Health Alliance (UHA) has updated its expedited review process to ensure members receive critical services as quickly as necessary when a delay could seriously jeopardize the member’s life, health, or ability to regain maximum function.
Clarification on Expedited Requests
Recently, UHA has received a growing number of expedited authorization requests that do not meet medical urgency criteria. Many of these requests were submitted for scheduling convenience or to speed approval after delayed provider submissions.
Effective immediately, any request submitted as expedited that is determined not to meet criteria for medical urgency will be reclassified as standard and processed under standard review timeframes.
Providers will receive notification when a request is reclassified.
Why This Matters
This change helps ensure that expedited reviews are reserved for members who face immediate health risks and that standard requests are processed efficiently for all others.
Provider Reminder
Before submitting an expedited request, confirm that:
- A delay in standard processing could seriously jeopardize the member’s health or function.
- Supporting documentation clearly explains the urgency.
- Routine or convenience-based requests are submitted as standard.
Updated Prior Authorization Rules for Lab Tests
Umpqua Health Alliance (UHA) has updated prior authorization (PA) requirements for several laboratory codes. These changes took effect November 1, 2025, and apply to all providers
| CPT / HCPCS Code | Description | Prior Authorization Requirement |
| 83993 | Assay for calprotectin, fecal | No PA required for any provider |
| 0485U | Oncology solid tumor, cfDNA and RNA, next-generation sequencing (NGS), genomic profile | PA required for all providers |
| 0211U | Oncology pan-tumor, DNA and RNA, genomic sequencing | PA required for all providers |
Updated HRSN Process Speeds Member Support
Umpqua Health Alliance (UHA) has implemented several changes to improve the efficiency and accuracy of Health-Related Social Needs (HRSN) request processing.
Turnaround Time
The processing timeframe for HRSN requests is now 28 days, with the option for an extension when necessary.
Fee Schedule Updates
Adjustments to the HRSN fee schedule have slightly increased the allowable costs for rent and utilities in our region.
Documentation Requirements
Requests for housing rent and utilities must include all required supporting documentation, such as:
- A signed lease
- Income verification
Incomplete requests will be dismissed. Members may resubmit once all required documents are provided.
Outreach and engagement providers are available to assist members with gathering the necessary documentation.
These updates are designed to reduce denials due to incomplete submissions and speed up processing for complete requests.
Supporting Members Through Transportation Updates
Umpqua Health Alliance (UHA) and Bay Cities Brokerage (BCB) have updated the Flex Transportation benefit, effective October 1, 2025.
These updates do not affect nonemergent medical transportation (NEMT). Members can still get rides to covered medical appointments. The changes apply only to nonmedical or “flex” rides, such as pharmacy, grocery, or community trips.
What Changed
- Pharmacy rides: Limited to one trip per month.
- DHS or WIC visits: Must show proof of appointment.
- Mental health hearings: Covered only for the member’s own case with proof of court date.
- Grocery stops: Allowed only when planned in advance and added to another approved appointment.
- UHA Community Advisory Council (CAC) or community meetings: Covered for members or invited guests with proof of meeting.
- Chadwick House rides: No longer covered.
- Gyms, Lamaze classes, equine therapy, and in-person weight loss programs: No longer covered. Online programs remain available.
- Self-help groups (NA or AA): May be limited; some members can receive a monthly bus pass instead.
New Support Options for Members
- Monthly bus passes: Available through BCB for members who take three or more covered rides per month. Passes may be mailed or picked up at Umpqua Transit.
- Online programs: Members can access weight loss and support group programs virtually.
- Grocery stops: Can still be included as part of another approved medical ride if planned ahead.
Members can find full details and additional resources on UHA’s Health Related Services – Flex Spending page here.
Care Coordination Supports Whole-Person Member Health
The Umpqua Health Alliance (UHA) Care Coordination Department brings together a multidisciplinary team of care navigators, medical care coordinators, HRSN coordinators, and behavioral health care coordinators. Together, they provide comprehensive support to ensure members receive the right care at the right time.
Recently, UHA implemented a Risk Stratification process to better identify member needs using a patient-centered, whole-person approach. A key component of this work is addressing Social Determinants of Health (SDoH)—the social and environmental factors that impact a member’s overall well-being.
Our Care Navigator Team is designed to identify and address SDoH early, before small challenges become major barriers to care. By collaborating with providers, Navigators help members access community resources and support for improved health and stability.
- Identifying Members
Members with low or no clinical risk scores—determined by claims data, predictive modeling, or prior assessments—are assigned to Navigators. The goal is early engagement, ensuring members receive support before issues escalate. - Outreach and Health Risk Assessment (HRA)
Navigators reach out by phone or mail to introduce themselves and offer assistance. With consent, they conduct an HRA that explores key SDoH domains such as:- Housing stability
- Food security
- Transportation
- Utilities
- Employment and financial strain
- Social support and safety
- Access to health care and medications
This assessment helps identify factors that may impact a member’s ability to maintain good health.
- Identifying Barriers and Prioritizing Needs
Care Navigators collaborate with members to determine which challenges to address first—prioritizing based on urgency and member preference. - Connecting to Community Resources
Members are linked to local community-based resources such as food pantries, housing programs, transportation services, and utility assistance.
Using trusted tools like Unite Us and verified internal resource lists, Navigators ensure referrals are local, accurate, and accessible. When possible, they provide a warm handoff to enhance follow-through. - Follow-Up and Continuous Support
Within one to two weeks, Care Navigators follow up to confirm successful connection and assess whether needs were met. Ongoing support continues until barriers are resolved.
Members with complex or high-risk needs are referred to a Care Coordinator for additional assistance. - Tracking and Quality Improvement
All interactions and outcomes are documented in UHA’s care management system. This data allows continuous monitoring of trends, resolution rates, and process improvements.
Why It Matters
Proactively addressing SDoH helps prevent avoidable health complications, increases member satisfaction, and strengthens community health.
How Providers Can Support This Work
- Encourage members to engage with their care navigator.
- Share insights on social or environmental challenges observed during visits.
- Refer patients who may benefit from non-clinical or community-based support.
Referral Information
To refer a member to UHA’s care coordination department:
Phone: 541-229-4842 (ask for the care coordination department)
Email: Casemanagement@umpquahealth.com
Fax: 541-229-8180
THW Connections Corner
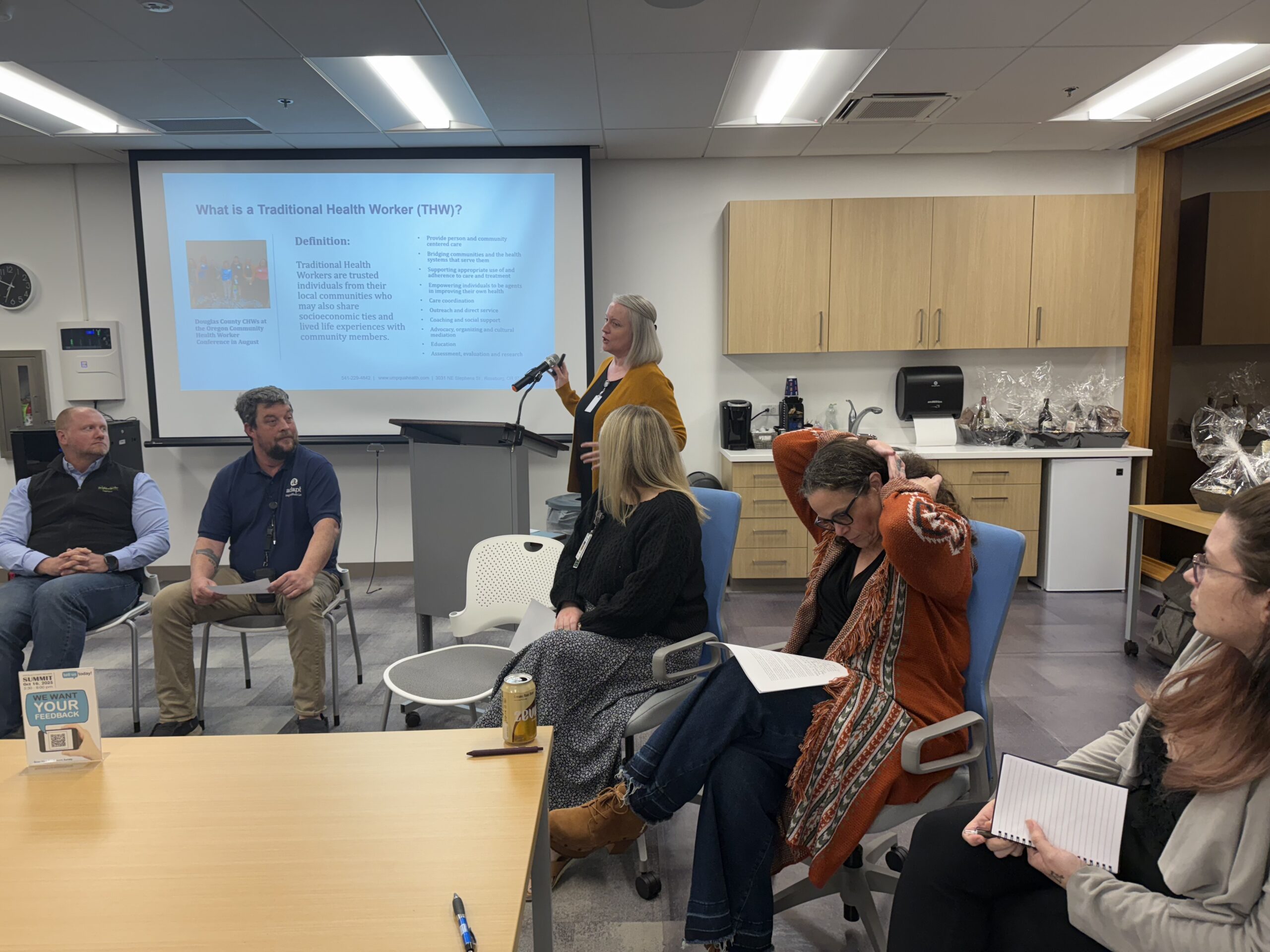
THWs Take Center Stage at Provider Summit
Event: Thursday, October 16, 2025
Focus: Traditional Health Workers (THWs) Q&A panel and community projects
Umpqua Health Alliance’s Traditional Health Worker (THW) liaison presented an overview of THW definitions and subtypes, the liaison role, and current community initiatives, including the THW Advisory Group, community health worker (CHW) curriculum development, the Health System Learning Collaborative, legacy clause promotion, and the THW newsletter.
The session featured a Q&A panel with community THWs who answered questions from the moderator and audience on navigating health systems, addressing disparities, and advancing health equity.
Panelists
- Wayne Ellsworth, CHW — Director of Resident Services, NeighborWorks Umpqua
- Cady Lyon, CHW — Director of Engagement, UCAN
- CeCe Lynn, CHW/PHN/Doula — Baby Beginnings / OHP, Evergreen
- Johnny Farmer, PSS/PWS/CRM — MH Crisis, Adapt Integrated Health Care
- Chriset Palenshus — Independent Doula, Herbnhood
- Aryn Voigt, PSS — Supportive Housing Peer Support Specialist, HIV Alliance Roseburg
- Sarah Swanson, CHW — Community Cancer Control Specialist, OHSU Knight Cancer Institute
Key Questions Discussed
- How can THWs help people navigate health care—especially those facing barriers?
- What roles do THWs play in reducing disparities and promoting health equity?
- How can policymakers, health leaders, and community members better support THWs?
Umpqua Health Alliance and the panel thank the organizers for the opportunity to share this work.

Get involved / Learn more:
Contact UHA THW Liaison Andrea Brown at abrown@umpquahealth.com.
CME for Thee
HPV and Oropharyngeal Cancer THW Training — Nov. 18
Date and Time:
Tuesday, November 18, 2025
3 to 5 p.m. PT
Location:
Live online training
Credits: 2 hours of continuing education
Presenter: Sarah Swanson, South Coast Community Cancer Control Specialist
Join the OHSU Knight Cancer Institute for a live, two-hour virtual training on the connection between human papillomavirus (HPV) and oropharyngeal cancers.
This session will provide tools and communication strategies for traditional health workers to promote HPV vaccination and discuss cancer prevention with patients and families.
Training Topics
- Understanding the link between HPV and oropharyngeal cancers
- The role of HPV vaccination in cancer prevention
- Strategies for discussing the HPV vaccine with families
- Communicating about HPV in culturally sensitive and respectful ways
Registration
Webinar: Language Access Workbook for Providers
Date and Time:
Tuesday, December 9, 2025
Noon to 1 p.m. PT
Location:
Zoom webinar
Audience: Providers, administrators, and staff involved in improving language access in health care
Join the Oregon Health Authority (OHA) and NORC at the University of Chicago for a one-hour webinar introducing Increasing Language Access in Oregon: A Workbook for Providers.
The workbook helps health care organizations and providers understand Oregon’s language access requirements and take practical steps to ensure patients receive care they understand. It offers strategies to meet state and federal standards, improve performance on the Meaningful Language Access (Health Equity) measure, and strengthen trust and communication with patients who prefer a language other than English or who use sign language.
During This Session, Presenters Will:
- Walk through the language access workbook and its key sections
- Share examples of how to use the workbook in everyday practice
- Discuss best practices for providing interpreter services
- Answer participant questions
Registration
Contacts:
Tania Curiel
Tania.V.Curiel@oha.oregon.gov
503-979-6980
Ilana Dickman
Dickman-Ilana@norc.org
Infectious Diseases Primer for Primary Care
The Department of Medicine, Division of Infectious Diseases at Johns Hopkins School of Medicine is offering a new Infectious Diseases Primer for Primary Care, an online course designed for primary care providers, residents, infectious disease fellows, hospitalists, and advanced practice providers.
This self-paced, eight-module course explores major infectious disease topics relevant to both outpatient and hospital settings. Participants will learn to identify, manage, and prevent common infections while promoting optimal patient outcomes.
Course Topics Include
- HIV management and antiretroviral therapy (ART) selection
- Screening, diagnosis, and treatment of latent tuberculosis
- Skin and soft tissue infections (bacterial, viral, fungal, and parasitic)
- Community-acquired pneumonia
- Vaccine updates
- Antibiotic stewardship
- Sexually transmitted infections (STIs)
Interactive case studies and clinical decision-making exercises help learners apply knowledge to real-world scenarios.
Learning Objectives
After completing this course, participants will be able to:
- Identify agents recommended for first-line ART and use antiretroviral decision-support tools.
- Describe screening, diagnosis, and treatment of latent tuberculosis infection.
- Recognize common skin infections and manage them effectively in primary care.
- Demonstrate understanding of antibiotic resistance, its drivers, and implications for clinical practice.
- Identify clinical presentations of common sexually transmitted infections and apply appropriate diagnostic and treatment strategies.
Learn More and Register
Clinical Corner
Coverage Change for Xifaxan Effective Oct. 1
October 1, 2025, Bausch Health and its subsidiaries, including Salix Pharmaceuticals, voluntarily withdrew from the Medicaid Drug Rebate Program (MDRP).
Under federal law, drug manufacturers must participate in the MDRP for their products to remain eligible for Medicaid coverage.
Because of this withdrawal, the Oregon Health Authority (OHA) Fee-for-Service (FFS) program can no longer cover Bausch Health products, including Xifaxan (rifaximin).
Key Impact
The greatest concern is for members currently using Xifaxan (rifaximin), as there are no generic equivalents or comparable alternatives available for certain members.
Recommended Provider Actions
To help maintain continuity of care for affected members, please:
- Identify and notify impacted members.
- Discuss future treatment plans.
- Consider therapeutic alternatives where appropriate.
- For members who must continue Xifaxan, assist them in applying for the Bausch Health Patient Assistance Program:
bauschhealthpap.com
HPV Vaccination: Protecting Patients From Preventable Cancers
Every day, physicians and care teams play a vital role in preventing disease and protecting community health. One of the most effective tools is the HPV vaccine—a proven way to prevent several types of cancer.
HPV Vaccination: Protecting Patients From Preventable Cancers
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. While many infections clear on their own, persistent HPV can cause:
- Cervical, anal, throat, penile, vulvar, and vaginal cancers
- Genital warts and precancerous lesions
Each year, more than 36,000 Americans are diagnosed with HPV-related cancers—most of which are preventable through vaccination.
A proven and safe prevention tool
The 9-valent HPV vaccine protects against the virus types responsible for nearly all HPV-related cancers and warts.
- Nearly 100% effective when given before exposure
- Extensively studied and monitored for safety
- Endorsed by leading health organizations worldwide
Who should receive the vaccine
- Ages 11–12: Ideal age to start (can begin at age 9)
- Ages 13–26: Catch-up vaccination for those not yet protected
- Ages 27–45: Consider vaccination through shared decision-making
Dose schedule:
- If started before age 15: Two doses, 6–12 months apart
- If started at 15 or older: Three doses for full protection
Supporting success in your practice
Small, consistent workflow changes can raise vaccination rates:
- EMR reminders for eligible patients
- Team-based education from nurses and medical assistants
- Follow-up calls or texts for dose completion
These actions not only boost vaccination coverage but also build trust and continuity of care.
Your recommendation matters most
Studies show that a provider’s strong recommendation is the single most important factor in a patient’s decision to vaccinate. HPV vaccination remains one of the most powerful cancer-prevention tools available today.
Updated Clinical Practice Guidelines Released
The Umpqua Health Alliance (UHA) Clinical Advisory Panel (CAP) meets quarterly to review and update clinical practice guidelines (CPGs) in alignment with current evidence and best practices
At its September 2025 meeting, the panel retired several CPGs and replaced them with updated advisories for the management of diabetes, hypertension, chronic obstructive pulmonary disease (COPD), and heart failure.
Access The Guidelines
All current CPGs are available on the updated UHA website:
Visit Umpqua Health Alliance Clinical Practice Guidelines page
Providers are encouraged to review these updates and integrate them into practice.
Submit Recommendations
Providers may submit additional recommendations to the Clinical Advisory Panel through the submission link on the same webpage.
WCHA Releases 2025–26 Immunization Guidance
The West Coast Health Alliance (WCHA) has released consensus immunization recommendations for the 2025–26 respiratory virus season. These guidelines have been endorsed by the Oregon Health Authority (OHA) and are intended to support provider decision-making during the upcoming respiratory season.
Background
Recent updates from the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) have generated discussion regarding timing, eligibility, and vaccine combinations for influenza, COVID-19, and respiratory syncytial virus (RSV).
The WCHA consensus statement provides clarity and regional alignment for immunization strategies across the West Coast.
Access The Recommendations
Both the ACIP and WCHA recommendations are available on the Umpqua Health Alliance website at the Clinical Practice Guidelines page:
Visit Umpqua Health Alliance Clinical Practice Guidelines page
Providers are encouraged to review the guidance and ensure that vaccine administration protocols align with these current recommendations.
Community Announcements
Connecting Douglas County to Food and Health
Access to healthy food is essential for good health — yet many Douglas County families face challenges putting nutritious meals on the table. To help bridge that gap, Umpqua Health Alliance (UHA) has launched a new Food Help page connecting members and community partners with local food pantries, meal sites, grocery discounts, and delivery options.
Food insecurity affects more than hunger. It influences chronic disease management, medication adherence, and overall wellness. The Food Help page gives providers and community organizations an easy way to connect patients with trusted, local resources.
Visit the page to explore resources and share with members who may need help accessing healthy food.
Visit Umpqua Health Alliance Food Help page
Together, we can make sure every family in Douglas County has access to nutritious food and the health that comes with it.
Network News
Umpqua Health Alliance Network Changes
Termed Providers and Facilities
- Alice Stappler, PA-C – PeaceHealth Medical Group September 30, 2025
- Brandi Myers, LPC – Centennial Medical Group September 6, 2025
- Carmel Townsend, DDS – Advantage Dental September 30, 2025
- Christine Huang, MD – PeaceHealth Medical Group September 30, 2025
- Janette Coelho Leal, MD – PeaceHealth Medical Group September 28, 2025
- Jennifer Mitchell, MD – PeaceHealth October 10, 2025
- Jermaine Goodell, CRM – Adapt Integrated Health Care October 16, 2025
Added Providers and Facilities
- Bo Bergeson, PHARM – PeaceHealth October 14, 2025
- Brian Delmonaco, MD – Roseburg Emergency Medicine October 1, 2025
- Daniel Young, PA-C – PeaceHealth August 12, 2025
- Emily Long, PA-C – PeaceHealth October 14, 2025
- Erin Johnson, LPC – PeaceHealth May 20, 2025
- Evan Tavakoli, MD – PeaceHealth July 9, 2025
- Garrett Brady, PA-C – PeaceHealth September 24, 2025
- Ian Hart, PA-C – PeaceHealth October 9, 2025
- Kevin Cummisford, MD – Anesthesia PC October 20, 2025
- Lisa Mai, PA-C – PeaceHealth October 14, 2025
- Lorraine Matice, CHW – Evergreen Family Medical September 29, 2025
- Malori Dixon, LPC – Adapt Integrated Health Care October 13, 2025
- Matthew Bzdega, MD – PeaceHealth May 1, 2025
- Michele Riggs, LCSW – PeaceHealth July 9, 2025
- Sabrina West-Hagberg, CHW – Evergreen Family Medical September 29, 2025
- Samir Ale, MD – PeaceHealth October 9, 2025
- Sonja Halvorson, PA-C – PeaceHealth September 19, 2025
- Stacy Goodwin, LPN – Adapt Integrated Health Care December 9, 2024
- Tonya Koonz, PA-C – PeaceHealth September 19, 2025
PT, OT, and ST Benefit Changes for 2026
Umpqua Health Alliance (UHA) is implementing changes to Physical Therapy (PT), Occupational Therapy (OT), and Speech Therapy (ST) benefits effective January 1, 2026.
Updated Visit Limits
Non-EPSDT members:
- Up to 8 visits per calendar year without prior authorization (in-network, above-the-line [ATL] providers)
EPSDT members:
- Up to 30 visits per calendar year (in-network, ATL providers)
Below-the-line (BTL) and out-of-network providers will continue to require prior authorization for all services.
These changes align UHA’s PT, OT, and ST coverage with current Oregon Health Plan (OHP) standards and are intended to support consistent access and administrative efficiency.
On the Lookout
Public Health History: The 1925 Serum Run to Nome, Alaska
Diphtheria is a serious bacterial infection that affects the respiratory system. It causes fever, nasal discharge, and a thick gray membrane on the tonsils and throat that makes it difficult to swallow and breathe. The diphtheria toxin can spread to other organs and be life threatening. Thanks to the DTaP vaccine, in the United States diphtheria is now very rare, with only a few cases per year from unvaccinated individuals who travel to other countries. Before the vaccine, diphtheria was a much-feared disease that caused suffocation and was generally considered a death sentence. Even with modern medicine today, the fatality rate for respiratory diphtheria remains between 5-10%, with higher death rates (up to 20%) for children under 5 and people over 40 years of age.
With this context, one can imagine the fear Dr. Curtis Welch must have felt in January 1925, when a three-year-old boy and seven-year-old girl died under his care with symptoms of diphtheria. Dr. Welch was working at Maynard Columbus Hospital in Nome, Alaska which had 975 settlers of European descent and 455 Alaska Native residents. Nome is a remote port town on the Bering Sea located two degrees south of the Arctic Circle. The treatment for diphtheria at the time was a horse-derived antitoxin, which greatly reduced mortality if administered early. But the serum supply at Dr. Welch’s hospital had all expired. On January 22nd 1925, he sent urgent telegrams to all major towns in Alaska and to the US Public Health Service requesting emergency assistance:
“An epidemic of diphtheria is almost inevitable here STOP I am in urgent need of one million units of diphtheria antitoxin STOP Mail is only form of transportation STOP I have made application to Commissioner of Health of the Territories for antitoxin already STOP There are about 3000 white natives in the district.”
The town of Nome went under quarantine while the governor of Alaska, the territorial board of health, and the US Public Health Service quickly organized a plan. There are no roads to Nome, the port was closed by ice, and severe storms made it too dangerous for planes to fly. The only way to deliver the needed medication was to use dog sled teams, a form of transportation historically relied on by the Native Athabascan people in this region of Alaska. The serum would only last six days under the freezing conditions of the trail, and every hour was needed to save the lives of the patients in the hospital. The 674-mile-long trip from the town of Sewart to Nome would typically take 30 days, so they organized a relay. A team of 20 mushers and 150 dog sled dogs raced across the Alaskan tundra and the shifting ice of the Bering Sea, passing the serum from team to team. It was a record freezing winter. The temperatures dropped below −50 °F, with a wind chill of −70 °F. The snow drifts were over 10 feet tall, and they mostly traveled in the dark due to the limited hours of daylight that time of year in the Arctic Circle. The sledders suffered frostbite in the blizzard conditions and many of the dogs collapsed and died.
On February 2, 1925, at 5:30 am, the musher Gunnar Kaasen completed the final leg of the journey and arrived in Nome. The serum made the 674 mile journey in a record-breaking 127.5 hours, or a little over 5 days. The medication was immediately thawed and given to patients. Not one of the vials were broken in the perilous journey. The mushers and Siberian husky dogs became a media sensation for their endurance and bravery, especially Balto, the dog that led the final leg of the journey, and Togo: the lead dog that completed the longest and most dangerous route. There is a statue of Balto in Central Park, New York City. Today, the annual Iditarod Dog Sled Race from Anchorage to Nome follows the same route to commemorate this history. “The Great Race of Mercy” is remembered by public health as a testament to determination, courage, and collaboration in providing care to rural frontier areas. The story helped raise awareness of the diphtheria vaccine and galvanized mass immunization across the United States.
Dental Digest
How Stress Affects Your Family’s Oral Health (and What to Do About It)
Life moves quickly. Between balancing work, school, family responsibilities and the unexpected curveballs that come our way, stress often becomes part of the daily routine. While most people know stress can affect things like sleep, energy levels or even heart health, fewer realize how it can impact oral health. Stress doesn’t just live in the mind. It shows up in the body, and often one of the first places it makes itself known is in the mouth.
At Advantage Dental+, we believe that caring for your family’s smiles means caring for the whole person – oral health may be our specialty, but full-body health from heart to mind is our focus. Understanding the connection between stress and oral health is an important step in protecting not only your teeth and gums, but also your overall well-being.

