Provider Newsletter – January 2021
 Practice Tactics
Practice Tactics
New Year, New Prioritized List
The Prioritized List of services for the Oregon Health Plan is updated and available here.
The funded lines continue at #1 through #471 for this year.
Request of Member Termination
There are times when a provider may request a member to be terminated and reassigned to a different Primary Care Provider (PCP). We would like to remind you that if you are terminating a UHA member from your practice, the Customer Care Department will need to be notified of the request. This is to provide the member with a smooth transition from your practice to a new PCP.
Depending on the nature for termination, UHA expects providers to consider, on an individual basis, whether termination would be appropriate for the member. If possible and safe to do so, providers should attempt to mitigate any behavior in order to maintain the relationship.
When a dismissal is necessary, please fax a copy of the letter to UHA Customer Care at 541-677-6038. This will ensure that we take the appropriate steps needed to provide our members with continued care while at the same time honoring the provider’s request of dismissal. The MS1 Corporate Policy is available to you by contacting the Customer Care Department at 541-229-4842 or by visiting our website at https://www.umpquahealth.com/provider-trainings/.
Maternal Fetal Monitoring Support Program
Improving pregnancy outcomes with outreach
UHA has partnered with OPTUM Maternity Support Program which provides outreach strategies and promotions to engage moms-to-be. With a focus on improving pregnancy outcomes, our program:
- Engages referred expectant mothers to drive participation
- Conducts risk assessments to identify and manage women at risk for preterm birth and other complications
- Provides personalized care and case management by experienced nurse case managers
- Offers a 24/7 BabyLine and portal to support members with questions about their pregnancy or newborn baby
- Provides comprehensive care and support to promote quality, cost-effective outcomes
- Reduces costly medical events
- Gives parents 24/7 access to RNs and more for up to six weeks after delivery
Managing high-risk pregnancies
Within our Maternity Support Program, our OB Risk Assessment and Education Program provides for the outreach, identification and case management of high-risk pregnant members. It reduces costly medical events and lowers the risk of NICU admissions and prolonged lengths of stay through four areas of focus:
- Enrollment — upon referral from provider
- Initial risk assessment — stratifies participants, provides targeted education and refers clinically appropriate participants to case management for additional support and resources
- Mid-pregnancy risk assessment — completed at 28 weeks’ gestation to identify complications for case management referral
- Outcome assessment and reporting — collects information following delivery, including labor and delivery, infant and maternal complications postpartum care
Collaborative case management
Once referred, high-risk pregnancies are connected to our OB Case Management. The OB case manager establishes a collaborative relationship that empowers the member and helps meet her needs through several avenues.
For all referral questions, please contact us at (541) 229-4842 or CaseManagement@umpquahealth.com.
Providers, if a member is high risk pregnancy or needs Maternal Fetal Monitoring, submit a PA referral for MFM and we will take care of the rest!
 Clinical Corner
Clinical Corner
The following is taken from a NEJM Journal Watch article:
December 28, 2020
Delabeling Penicillin Allergy
David J. Amrol, MD, Associate Professor of Medicine and adjunct Assistant Professor of Pediatrics at the University of South Carolina School of Medicine
Most patients with recorded penicillin allergy actually are not allergic.
Penicillin allergy is noted in the records of more than 10% of the U.S. population; however, most patients have either “outgrown” their allergy or actually experienced viral rash or non-immunological adverse reactions such as diarrhea. Penicillin allergy is associated with patients receiving more-expensive, less-effective, and more-toxic antibiotics (NEJM JW Gen Med Aug 1 2020 and JAMA Intern Med 2020; 180:1120). Several studies published during the past year inform efforts to “delabel” patients who are incorrectly labeled as penicillin allergic.
Penicillin skin testing has a very good negative predictive value, but it is not widely available and has a high false-positive rate. In low-risk patients, observed oral challenge is a safe alternative (NEJM JW Gen Med Oct 15 2019 and J Allergy Clin Immunol Pract 2019; 7:2163). To help define “low risk,” researchers conducted a review of 447 patients and determined that those with “benign rash” longer than 1 year ago — and without angioedema, mucosal involvement, or systemic symptoms — could skip skin testing and proceed directly to oral challenge. Of the 55% of patients who met these criteria, >97% tolerated oral challenge (NEJM JW Gen Med Mar 15 2020 and J Allergy Clin Immunol Pract 2020; 8:681).
In a separate study, researchers validated the clinical decision tool called PEN-FAST using skin tests, challenges, or both in 945 patients with reported penicillin allergy. Patients received 2 points for an event in the previous 5 years, 2 points for anaphylaxis/angioedema or severe cutaneous adverse reaction, and 1 point for a reaction requiring treatment. Half of patients were low risk (defined by a score <3), and only 4% of patients had positive skin tests or oral challenges. The resulting negative predictive value was 96% (NEJM JW Gen Med Apr 15 2020 and JAMA Intern Med 2020; 180:745).
Often, reviewing history alone (statements such as, “Augmentin caused diarrhea”) is enough to remove an allergy diagnosis. When patients make statements such as “I had a rash with amoxicillin 20 years ago,” I just give 500 mg of amoxicillin and observe for 2 hours in my allergy practice. I reserve penicillin skin testing for those with plausible IgE-mediated reactions such as angioedema, anaphylaxis, or sudden onset of urticaria, especially within the past 5 years. If a patient reports a severe cutaneous reaction such as Stevens-Johnson syndrome, drug reaction with eosinophilia and systemic symptoms (DRESS), serum sickness, or acute generalized pustulosis, then skin testing is not helpful, and lifelong avoidance of penicillin is warranted.
 On the Lookout
On the Lookout
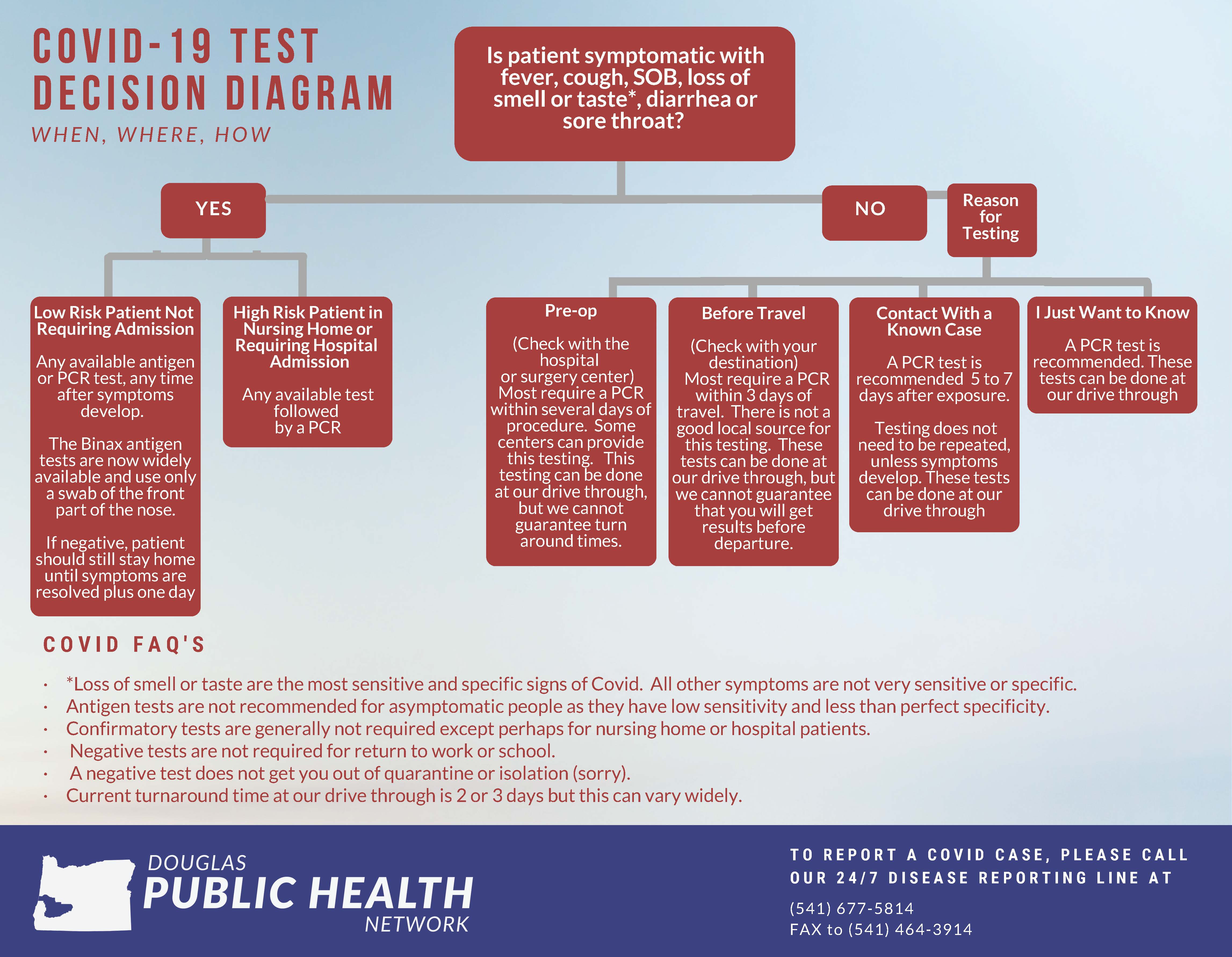
The Douglas Public Health Network provided an excellent decision tree for management of COVID-19 testing at this decision tree, as well as a patient information handout for isolation and quarantine.
Information on DPHN’s role in COVID vaccination is forthcoming; link to their website: http://douglaspublichealthnetwork.org/
 CME for Thee
CME for Thee
COVID-19 information sessions for providers
Thank you for your leadership and partnership in helping to slow the spread and address the health impacts of COVID-19 in Oregon. With this rapidly changing situation, we want to get information out to healthcare providers across the state as quickly and clearly as possible. To provide a consistent venue for COVID-19 information sharing, OHA’s Chief Medical Officer, Dana Hargunani, M.D., will host regular information sessions for Oregon health care providers. Recordings of past sessions are available here: https://www.oregon.gov/oha/PH/DISEASESCONDITIONS/DISEASESAZ/Pages/COVID-19.aspx
Informational sessions for all health care provider: 1st and 3rd Thursdays, noon-1 p.m.
Links for upcoming sessions:
- January 7: https://join-noam.broadcast.skype.com/dhsoha.state.or.us/46f5aacd5f564ac3a828fc48e5560861
- Meeting recordings: https://www.oregon.gov/oha/covid19/Pages/Healthcare-Partners.aspx (scroll down to “OHA COVID-19 Healthcare Provider Webinars”)
REALD learning series
The OHA Transformation Center and Division of Equity and Inclusion hosted a webinar series focused on the use of REALD (race, ethnicity, language and disability) for CCOs, clinics and other health care leaders. REALD is an effort to increase and standardize race, ethnicity, language and disability data collection across DHS and OHA. Recordings of all webinars in the series are available here: https://www.oregon.gov/oha/OEI/Pages/REALD.aspx
Trauma-Informed Care for Health and Allied Professionals ECHO Program
January 13 through March 31, 2021 https://www.oregonechonetwork.org/traumainformedcare
OPAL-C: a peer support resource available to medical providers in Oregon during COVID-19
The Oregon Psychiatric Access Line (OPAL) would like to announce a new service for its callers, OPAL-C (COVID-19 Clinician Stress Peer Support). In addition to offering psychiatric curbside consultations about adult and child patients, OPAL is now offering confidential peer support for primary care clinicians experiencing stress in response to the COVID-19 crisis for the next 12 months. OPAL consultants will provide a listening ear and suggestions for managing the stress that comes from this national emergency. In addition, OPAL consultants can provide information regarding available community-based resources for practitioners seeking to establish care with a mental health professional.
So, if you are interested in talking about COVID19 practice stress, feel free to call the regular OPAL number 503-346-1000 or toll free 855-966-7255 for out of Portland Metro. Please let call receptionist know of your desire to talk about COVID-19 related stress issues.