Practice Tactics
Communicating Through the CIM Portal
When notes are added to a prior authorization request in the CIM Provider Portal, they do not automatically generate a notification to the Umpqua Health Alliance prior authorizations team. As a result, messages entered only as notes may not be seen in a timely manner.
To ensure communication is received and reviewed, providers should use the portal’s email functions when sending messages related to prior authorization requests.
How to Ensure Your Message Is Received
- For new messages: Use the email function within the CIM Provider Portal to send a message directly to the prior authorizations team.
- When replying to an email: If responding to an email received through the portal, use the Reply or Reply All function. These options are available by selecting the three dots located on the right side of the email note.
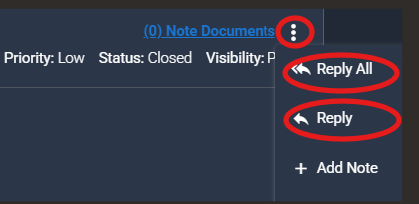
Using the email functions within the portal helps ensure questions, clarifications and updates are routed appropriately and addressed without delay.
Why Was My Prior Authorization Denied?
Key Authorization Policies
Common Reasons for Prior Authorization Denials:
Chiropractic Care
Chiropractic services are subject to specific coverage criteria. Denials most often occur when one or more of the following requirements are not met:
- A referral from a primary care provider or specialist is required.
- The referring provider’s evaluation must be conducted in person and within 60 days of the referral.
- Members may not be referred to more than one therapy at the same time, including physical therapy, chiropractic care or acupuncture.
- Chiropractic services are covered only for conditions of the spine.
- The maximum number of visits for a single condition is 30 per year across all therapies combined.
- Treatment courses are generally limited to eight weeks. Maintenance chiropractic care is not supported by evidence and is not covered.
Additional information about the Prioritized List and coverage criteria is available through the Oregon Health Authority.
How to Appeal a Denied Request
Members have the right to appeal a denied service by following the instructions included in their denial notice. Appeal instructions are also available on the Umpqua Health Alliance website and must be followed to ensure timely review.
An appeal must be requested within 60 days of the date on the denial notice. Appeals may be requested by the member or the provider/authorized representative with written permission of the member.
How to Request an Appeal
Appeals may be submitted using one of the following methods:
- By phone: Call during business hours at (866) 672-1551.
- TTY: Dial 711 or (541) 440-6304.
- In writing: Complete the Request to Review a Health Care Decision form (OHP 3302), which is included with the denial notice. Return the completed form by mail or fax using the contact information below.
Mail:
Grievance and Appeals
3031 NE Stephens St.
Roseburg, OR 97470
Fax: (541) 677-5881
Providers may assist members by completing the OHP 3302 form and obtaining the member’s signature. The completed form should be submitted by fax. When a denial has occurred within the past 60 days, this appeal process should be used instead of submitting a duplicate request for the denied service.
Recent Benefit Plan Updates
Several benefit plan updates affecting coverage and prior authorization requirements are now in effect. Providers are encouraged to review the changes below to ensure accurate billing and appropriate use of services.
| Code | Description | Effective Date | Prior Authorization |
| G0279 | Tomosynthesis, mammography | Jan. 1, 2026 | No PA required for any provider |
| 43762 | Replacement of gastrostomy tube without revision of tract | Jan. 1, 2026 | No PA required for any provider |
| J0878 | Daptomycin injection | Dec. 12, 2025 | No PA for in-network providers; PA required for out-of-network providers |
| 99201 | Office or other outpatient visit, 10 minutes | Removed Jan. 21, 2026 | Code deleted by AMA and CMS effective Jan. 1, 2021 |
Notes for Providers
- The removal of 99201 reflects national Evaluation and Management coding changes and should no longer be used for billing.
- Providers should update internal coding references to reflect these changes and avoid claim denials or delays.
Skilled Nursing Facility Coverage Update
The Oregon Health Authority has updated the maximum covered length of stay for skilled nursing facility services to align with Medicare guidelines. When medical necessity criteria are met, members may now receive covered skilled nursing facility care for up to 100 days.
Coverage determinations for skilled nursing facility services are based on clinical criteria outlined in Oregon Administrative Rule 411-070-0033 and InterQual guidelines. These criteria are used to assess the appropriate level of care and ongoing medical necessity throughout the stay.
Providers should continue to assess members regularly and ensure documentation supports the need for skilled nursing facility services for the duration of care.
HRSN Medically Tailored Meals Overview
Medically tailored meals are designed to support members with specific health-related conditions for which targeted nutrition interventions may improve health outcomes. Eligible members may receive up to three meals per day for a period of up to six months as part of the Health-Related Social Needs benefit.
To qualify for medically tailored meals, members must meet all eligibility requirements outlined below.
Medically Tailored Meals Eligibility
- The member must be part of a Health-Related Social Needs covered population.
- The member must have at least one qualifying health condition.
- The member must be experiencing low or very low food security, as measured by the U.S. Household Food Security Survey Module: Six-Item Short Form from the U.S. Department of Agriculture. These questions are included in the HRSN application for this benefit.
- A nutrition care plan is required and must include medically tailored meals and the specific nutrients required.
- Complete eligibility criteria are outlined in Oregon Administrative Rule 410-120-2005, including HRSN service eligibility, identification of eligible members, and outreach and engagement requirements.
In situations where a member meets eligibility criteria but the primary care provider is unable to complete the required nutrition care plan, additional support options are available.
Members or providers may submit a completed HRSN nutrition request for medically tailored meals. Providers may assist members by helping obtain the required nutrition care plan assessment prior to application submission. If needed, Umpqua Health Alliance can refer eligible members to contracted registered dietitians to complete the nutrition care plan assessment.
Additional training and guidance on the medically tailored meals benefit are available through the provider training materials on the Umpqua Health Alliance website.
THW Connections Corner
Rural Community Health Worker Peer Meet-Up
A monthly virtual peer meet-up is available for Rural Community Health Workers working across Oregon.
The meet-up provides a space for CHWs to connect with peers, share resources and exchange strategies related to community-based care in rural settings. Discussions are participant-driven and focus on practical challenges, lessons learned and opportunities for collaboration.
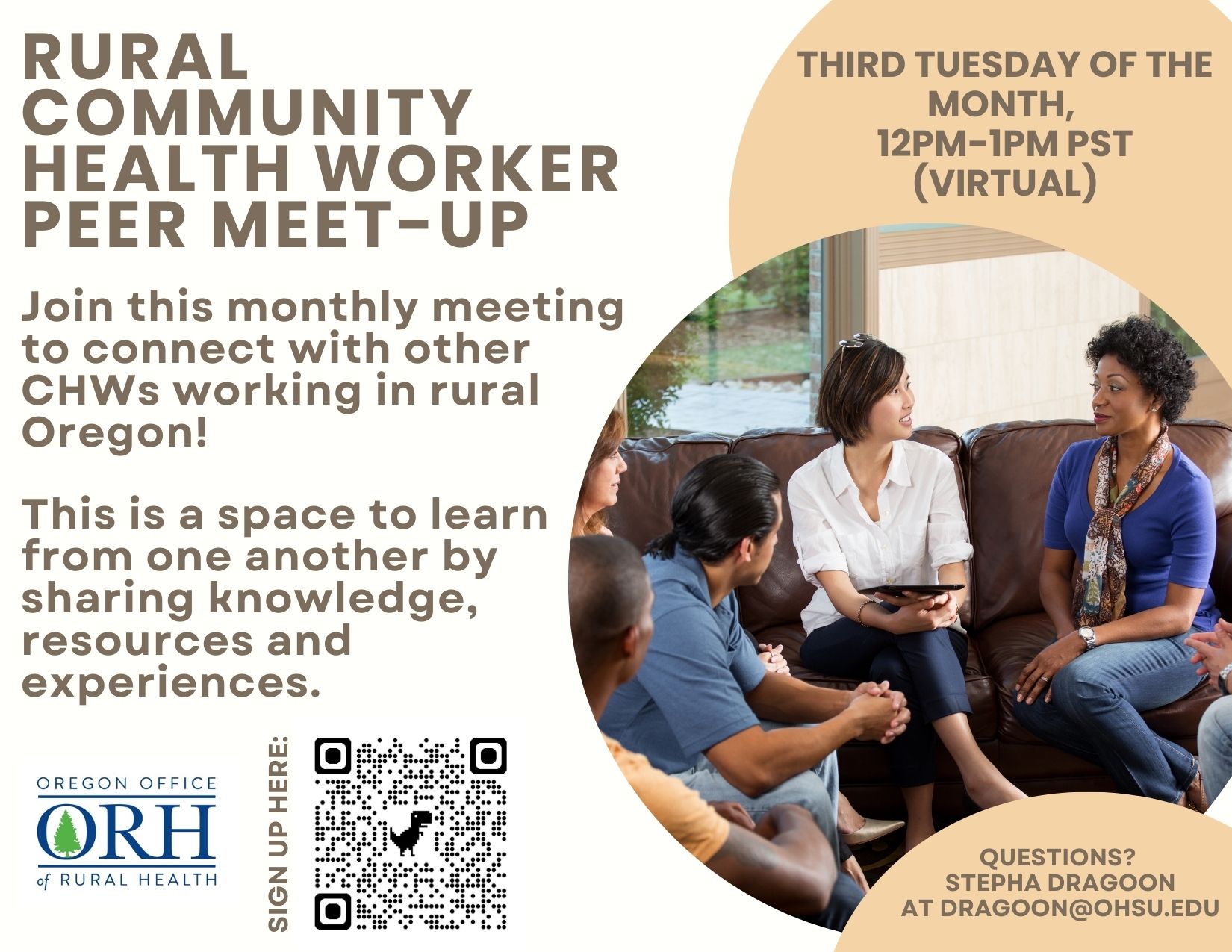
The meet-up is held virtually on the third Tuesday of each month from noon to 1 p.m. PT.
Advocacy Day at the Oregon State Capitol
Advocacy Day is an in-person event that brings together community partners to highlight priorities affecting health, recovery and prevention services in Oregon.
The event focuses on policy areas related to Medicaid, peer-based services, recovery housing, care during incarceration, adolescent and family services, recovery high schools and primary prevention. Participation is optional and intended for individuals interested in systems-level awareness and advocacy.
Advocacy Day will be held Thursday, Feb. 12, from 7:30 a.m. to 3:30 p.m. at the Oregon State Capitol in Salem.
How THWs Advance Health Equity
Traditional Health Workers (THWs) play an important role in putting equity into action across care teams and communities by addressing barriers that affect access to care and health outcomes.
Equality means offering the same resources to everyone. Equity recognizes that people experience different barriers to care and may need different levels of support to achieve similar health outcomes. In practice, equity focuses on access, trust and responsiveness to individual and community needs.
Traditional Health Workers work directly with individuals and families to identify barriers that may not surface in a clinical setting. These barriers can include transportation challenges, language access, housing instability, limited health literacy or past experiences that have reduced trust in health systems.
By design, THWs address these challenges through culturally responsive outreach, relationship-building and navigation support. Their lived experience, community knowledge and sustained engagement help ensure care plans are realistic, accessible and aligned with what matters to the member.
Providers may refer members to THW services through the Umpqua Health Provider Directory. You can also reach out to Andrea Brown, THW Liaison with Umpqua Health Alliance at abrown@umpquahealth.com if you have questions about which THW type might be a good fit for the members you serve.
THW Equity-related work is shared with the Oregon Health Authority in our annual Traditional Health Worker integration and utilization reporting.
Once a referral is made, providers are expected to follow up with the member and the THW to ensure effective collaboration and continuity of care.
For providers, integrating THWs into care teams strengthens care coordination, improves follow-through, and supports more equitable outcomes. Equity is not achieved by treating everyone the same. It is achieved by meeting people where they are and responding to what they need to engage in care.
Traditional Health Workers help make that possible.
CME for Thee
Suicide Prevention Trainer Opportunities
Suicide prevention training expands early identification, culturally responsive intervention and community-based support for members at higher risk. These no-cost, virtual opportunities prepare Traditional Health Workers and community partners to deliver evidence-based trainings across Oregon.
The following trainer programs are available in 2026.
Question, Persuade, Refer Training for Trainers
This program prepares participants to deliver suicide prevention trainings in community settings. It is offered by Lines for Life in partnership with the Oregon Health Authority.
- Who it is for: THWs and community partners working in youth-facing settings, with veterans, or with culturally specific communities, including individuals able to train in languages other than English
- Commitment: Deliver multiple trainings each year and participate in a monthly trainer learning collaborative
- Key dates: Feb. 25 and March 31, 2026
- Learn more or apply: Full program details and application information are available through Lines for Life
Be Sensitive, Be Brave Trainer Academy
This trainer academy offers certification to deliver suicide prevention and mental health trainings with a focus on culturally responsive engagement.

- Who it is for: THWs, educators, bilingual trainers and individuals working with youth or adults at increased risk of suicide
- Commitment: Complete a multi-session virtual academy, deliver multiple trainings each year and participate in ongoing learning activities
- Key dates: February, June and November 2026 academies
- Learn more or apply: Full program details and application information are available through Lines for Life
Youth SAVE Virtual Training of Trainers
This training prepares participants to deliver Youth SAVE suicide prevention programming focused on youth and peer engagement.
- Who it is for: Individuals working closely with youth in community or educational settings
- Commitment: Attend a two-day virtual training; full participation is required
- Key dates: Feb. 26–27, 2026
- Learn more or apply: Application and information session details are provided by Youth SAVE
Motivational Interviewing Training on Immunization
Free virtual and in-person trainings on motivational interviewing are available for health care providers and immunizers.
Motivational interviewing is an evidence-based approach that supports patient-centered conversations and shared decision-making around health behaviors, including immunization. These trainings are sponsored by the Oregon Health Authority Transformation Center in partnership with Boost Oregon.
The trainings focus on practical communication strategies for addressing vaccine hesitancy, building trust and supporting informed decision-making across diverse populations.
Virtual training: Addressing vaccine hesitancy
This one-hour webinar introduces the underlying philosophy and core skills of motivational interviewing as they apply to vaccine conversations. Participants will learn how using open questions, affirmations, reflective listening and recognizing autonomy can foster trust and collaboration. The session will also cover the Ask-Offer-Ask framework for sharing vaccine information in a way that respects choice and encourages meaningful dialogue.
Date: Wednesday, Feb. 25, noon–1 p.m.
Facilitator: Carrie Bader, MPH, training director at Boost Oregon.
Virtual training: Vaccine conversations across cultures
This one-hour virtual session reviews culture-based reasons for vaccine hesitancy, including historical trauma, religious practices and political beliefs. Participants will learn how to approach these conversations respectfully and how to use motivational interviewing skills to promote vaccination in a culturally sensitive manner.
Dates: Wednesdays, March 11 and March 18, noon–1 p.m.
Facilitators: Carrie Bader, MPH, training director at Boost Oregon, and Caroline Nguyen Ticarro, executive director at Boost Oregon.
Registration: March 11 and March 18
In-person, full-day workshops
In-person trainings will be held in Portland, Medford and Bend in spring 2026. These six-hour workshops will offer continuing medical education credit through the American Academy of Family Physicians. Dates and locations will be posted to OHA’s CCO metrics technical assistance webpage for child and adolescent immunizations.
Improving Colorectal Cancer Screening
Oregon Rural Practice-based Research Network is offering a free, two-part webinar series to support rural clinical practices in improving colorectal cancer screening through patient outreach strategies. This training is focuses on practical approaches to increase screening rates using evidence-based methods.
Colorectal cancer is the second leading cause of cancer-related death in the United States. Strategies such as mailing fecal immunochemical tests and providing patient navigation support have been shown to increase screening and early detection, particularly among diverse and underserved populations.
Participants will learn how to provide adults with an at-home colorectal cancer screening option, design an outreach program using best available evidence, and understand the return on investment and organizational benefits associated with screening outreach.
Two-Part Webinar Series
- Dates: Wednesday, Feb. 25, and Wednesday, March 4
- Time: Noon–1 p.m.
- Cost: Free
- Registration: https://us02web.zoom.us/meeting/register/grz-Dd9zRVehNJMaUklM-A#/registration
- Contact: smartercrc@ohsu.edu
Clinical Corner
Immunizations for Children: Provider Guidance
Vaccination remains one of the most effective public health strategies for preventing serious illness, reducing hospitalizations and protecting community health. Providers play a critical role in offering clear, evidence-based recommendations and addressing patient and family questions with confidence.
Changes in national vaccine guidance have caused confusion about who should receive vaccines and when. In response, Oregon has joined the West Coast Health Alliance to ensure public health guidance is based on science and evidence. Oregon remains committed to science-driven public health policy.
The Oregon Health Authority supports vaccination recommendations from the American Academy of Pediatrics, the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists. Guidance from these organizations is incorporated into Oregon’s Model Immunization Protocols and reflects current clinical best practices.
At the time of publication, the coordinated care organization metrics related to childhood and adolescent immunizations have not changed.
Required Immunizations for School and Child Care
In Oregon, school immunization requirements are unchanged for the 2025–26 school year. School immunization requirements are established at the state level and are independent of federal recommendations. Oregon continues to recommend that children receive all vaccines recommended by the American Academy of Pediatrics in accordance with the routine immunization schedule.
Providers should continue to follow Oregon’s immunization requirements when completing school and child care documentation and advising families on compliance.
Recommended Immunizations Not Required for School
In addition to school-required vaccines, the American Academy of Pediatrics continues to recommend pneumococcal conjugate, human papillomavirus and meningococcal vaccines as part of routine preventive care.
The pneumococcal conjugate vaccine is recommended as a four-dose series at 2, 4, 6 and 12–15 months of age. The American Academy of Pediatrics recommends starting the human papillomavirus vaccination series for children between ages 9 and 12. The meningococcal vaccine is recommended in two doses, with the first dose at ages 11–12 and a booster dose at age 16.
While these immunizations are not required for school attendance, they remain recommended. Providers are encouraged to continue discussing these vaccines with families and offering them according to the routine immunization schedule.
Immunization Support for Providers
Conversations about vaccines and vaccine-preventable diseases are increasing in clinical settings as families navigate changes in national guidance. Providers seeking additional support are encouraged to connect with the Douglas Public Health Network.
Douglas Public Health Network can provide copies of the immunization schedules followed by the Oregon Health Authority and the American Academy of Pediatrics, as well as patient-facing materials to support informed, respectful dialogue. The organization also offers training and resources on evidence-based communication approaches, including motivational interviewing, to assist providers in addressing questions and concerns during this evolving and sometimes confusing time for patients and families.
Umpqua Health Alliance values its partnership with providers in supporting the health of members and communities and is committed to removing barriers to preventive care. These immunizations remain covered benefits for Umpqua Health Alliance members and are available at no cost. Umpqua Health Alliance aligns with the Oregon Health Authority in supporting evidence-based vaccination guidance from trusted medical organizations and appreciates providers’ role in delivering consistent, science-based care. Providers with questions or needing additional support are encouraged to reach out for assistance.
Continuous Glucose Monitor Coverage and Authorization
A continuous glucose monitor is a wearable medical device used to measure glucose levels throughout the day and night. Continuous glucose monitors provide near real-time glucose readings and reduce the need for routine fingerstick blood glucose testing.
Continuous glucose monitors use a subcutaneous sensor to measure glucose concentrations in interstitial fluid. Glucose data are transmitted to a compatible receiver or mobile device. These devices support diabetes management by displaying glucose trends and patterns and by providing alerts for hyperglycemia and hypoglycemia, which may help reduce glycemic variability and improve patient safety.
All continuous glucose monitors require prior authorization. Providers should submit prior authorization requests to Umpqua Health Alliance.
Before approval of an initial prior authorization, members must receive education on continuous glucose monitor use and meet one of the following criteria.
Type 1 diabetes and one of the following
- Age 20 years or younger
- Pregnancy
- Adult using an insulin pump
- Hemoglobin A1c of 8.0% or higher
- Recurrent hypoglycemia
- Hypoglycemia unawareness
Type 2 diabetes
Members must be using short- or intermediate-acting insulin multiple times daily and have at least one of the following:
- Hemoglobin A1c of 8.0% or higher
- Recurrent hypoglycemia
- Hypoglycemia unawareness
- Diabetes-related complications, including neuropathy or organ damage
Prior Authorization Duration and Renewal Requirements
Initial authorizations
- Continuous glucose monitor device: Approved for two years
- Continuous glucose monitor sensors: Approved for six months
Renewal authorizations
- Continuous glucose monitor device: Approved for two years
- Continuous glucose monitor sensors: Approved for one year
Approval of a continuous glucose monitor sensor renewal requires:
- An in-person or telehealth visit with the prescribing provider every six months following the initial prescription, and
- Documentation demonstrating the member has used the continuous glucose monitor device for at least 50% of the time since the most recent provider visit
Providers should ensure clinical documentation supports ongoing medical necessity and device utilization when submitting renewal requests.
CGM Fulfillment Options
Continuous glucose monitors may be obtained through:
- Retail pharmacies, or
- Durable medical equipment providers
Provider Support
Umpqua Health Alliance is committed to supporting providers and members in accessing appropriate diabetes management tools. For additional information about continuous glucose monitor coverage or submitting prior authorizations, visit
https://www.umpquahealth.com/providers/health-plan-services/prior-authorizations/.
New Rheumatology Resource Added Online
A new Rheumatology resource has been added to the Clinical Practice Guidelines webpage under the Pharmacy section. This update is intended to support provider access to rheumatology-related pharmacy resources in a centralized location.
The new button links to a rheumatology pharmacy presentation that includes an overview of major rheumatologic conditions, treatment guidelines, and newer therapies introduced within the past five years. The material is organized as a reference and may be helpful for providers involved in prescribing, medication management or care coordination for members receiving rheumatologic therapies.
This resource is available on the Umpqua Health Alliance website and is provided for informational purposes.
- Rheumatology Pharmacy Resource:
https://www.umpquahealth.com/wp-content/uploads/2026/01/dmards-review-en.pdf
Community Announcements
Ongoing Community Wellness Activities
Supporting prevention and long-term condition management often extends beyond what can be addressed during an office visit. Regular movement, stress regulation and opportunities for social engagement can play a role in sustaining progress between encounters. Community programs offer a practical way to bridge clinical guidance with daily routines. The ongoing activities described here are free, locally available and designed for consistent participation. These options can be aligned with care plans when community-based support is appropriate.
Mindful Movement Wednesdays
This weekly, in-person class offers a structured opportunity for gentle movement and stress reduction. Providers may share this activity with members seeking low-impact physical activity or mindfulness-based support.
- When: Wednesdays, noon–1 p.m.
- Where: The Vortex Center, 865 SE Court Ave.
- Cost: Free
Cow Creek Health and Wellness Walking Group
This recurring walking group combines physical activity, social connection and informal nutrition discussion. Providers may consider this option for members who benefit from routine movement and peer support in an outdoor setting.
- When: Second and fourth Tuesdays of the month, 9–10 a.m.
- Where: Millsite Park, Myrtle Creek; meet at the covered bridge at the southeast end of the park
- Who: Open to all community members
- Contact: Claire Grubb, RD, at (541) 672-8533, ext. 5266

Printable versions of these resources are available for distribution in clinical settings. To request PDF files, contact deverson@umpquahealth.com.
Nutrition-Focused Community Events
Nutrition counseling is most effective when members are able to apply guidance in everyday settings. Translating recommendations related to food choices, budgeting and meal preparation can be challenging without opportunities for hands-on practice. Skill-based learning experiences can help bridge that gap by reinforcing concepts discussed during visits. The nutrition-focused events described here emphasize practical strategies that align with preventive care and chronic disease management. These options may be useful when additional, applied nutrition support would add value.
Cow Creek Grocery Shopping Tour
This guided grocery store tour focuses on navigating food options, comparing products and making budget-conscious choices. It may be appropriate for members who benefit from real-world nutrition guidance and increased confidence with everyday shopping decisions.
- When: Feb. 26, 8–9 a.m.
- Where: Sherm’s Thunderbird Market, Roseburg
- Contact: (541) 672-8533, option 2

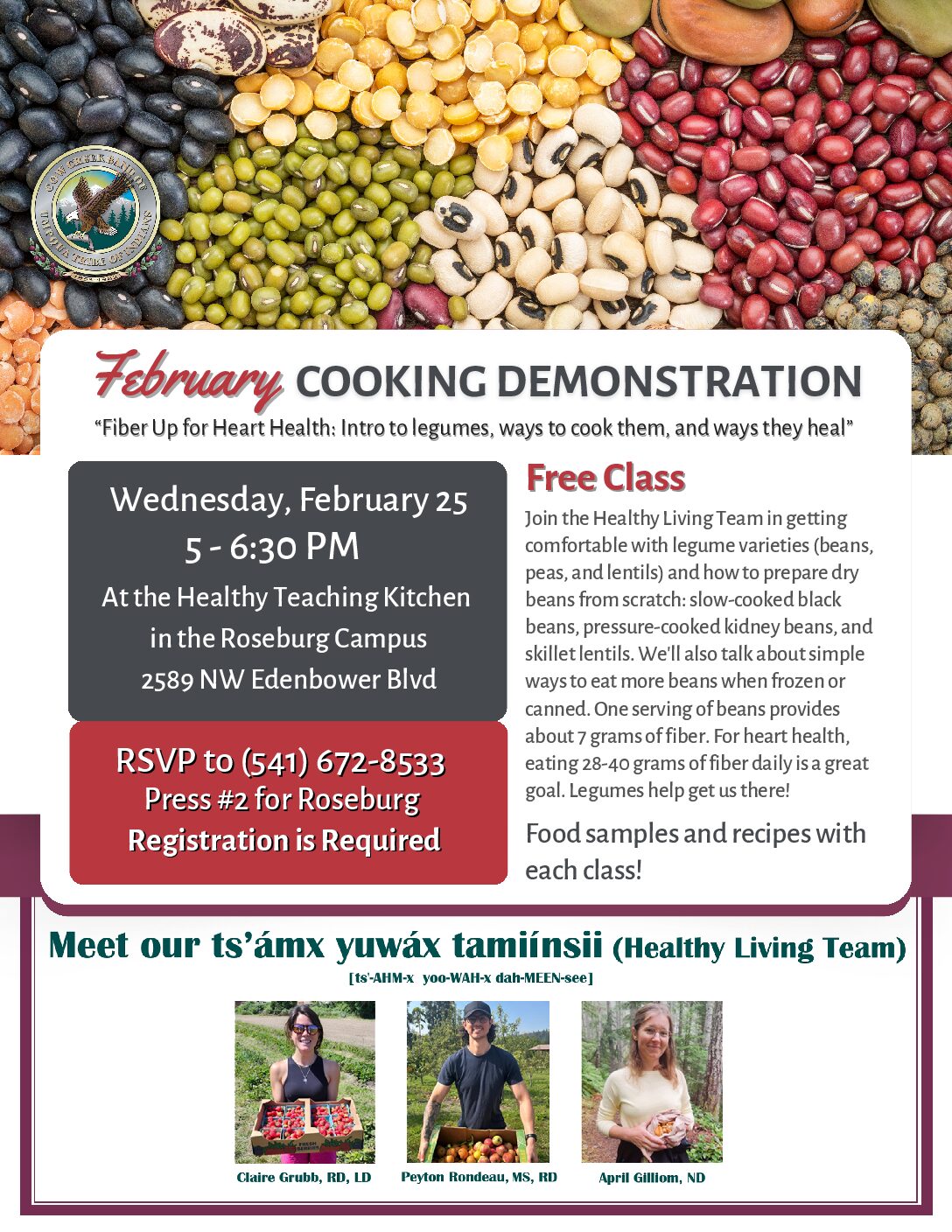
Cow Creek Cooking Demonstration
This free, in-person cooking demonstration focuses on increasing fiber intake through legumes and includes practical preparation techniques, recipes and food samples. It may be appropriate for members interested in heart health, diabetes prevention or building basic cooking skills to support nutrition goals.
- When: Wednesday, Feb. 25, 5–6:30 p.m.
- Where: Healthy Teaching Kitchen, Roseburg campus, 2589 NW Edenbower Blvd.
- Registration: Required
- Contact: (541) 672-8533, press 2 for Roseburg
Printable PDF versions of these materials are available for use in clinical settings. To request copies, contact deverson@umpquahealth.com.
Diabetes Self-Management Education and Support
Effective diabetes management often requires ongoing education and reinforcement beyond routine office visits. Some members benefit from structured support that combines skills-based learning with individualized guidance over time. Diabetes Self-Management Education and Support offers an organized approach to reinforcing treatment plans, nutrition goals and self-care behaviors. The program integrates group education with one-on-one support from trained educators. It may be appropriate when additional education and sustained follow-up would support effective diabetes management.
Diabetes Self-Management Education and Support (DSMES)
This six-week program provides education and tools to help members manage diabetes and related conditions. The program combines group workshops with individual sessions that include medical nutrition therapy or diabetes education. It is available in English and Spanish and is accredited by the Association of Diabetes Care and Education Specialists.
- Format: Group education and individual sessions
- Duration: Six weeks
- Languages: English and Spanish
- Coverage: Covered by Medicare and Medicaid in Oregon
- Contact: (833) 673-9355
- Learn more: https://hipaa.jotform.com/223126536395155
Additional diabetes resources for members are available at
https://www.umpquahealth.com/members/benefits-programs/diabetes-prevention-management
Printable version of this resource is available for distribution in clinical settings. To request PDF file, contact deverson@umpquahealth.com.
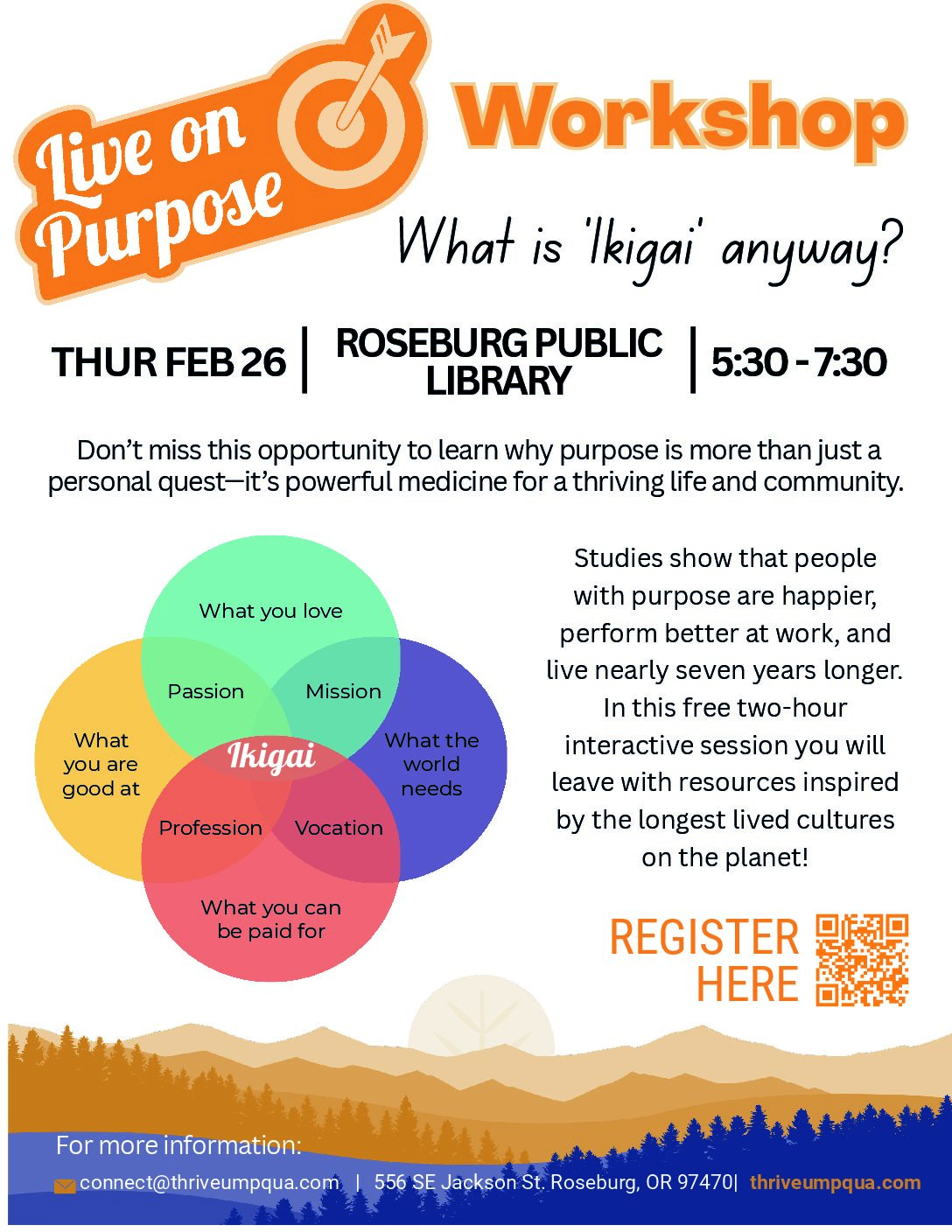
Live on Purpose Community Workshop
Some members seek additional support related to stress, motivation or overall well-being that falls outside formal treatment plans. Short, single-session workshops can offer an opportunity for reflection and discussion without requiring ongoing participation. The workshop described here focuses on purpose, resilience and personal well-being. It is designed as a standalone experience rather than a clinical intervention. This option may be relevant when members ask about brief or exploratory support opportunities.
This free, in-person workshop introduces concepts related to purpose and well-being and draws on examples from long-lived cultures. The session is designed to encourage reflection and discussion in a group setting.
Live on Purpose Workshop
- When: Thursday, Feb. 26, 5:30–7:30 p.m.
- Where: Roseburg Public Library
- Address: 556 SE Jackson St., Roseburg, OR 97470
- Cost: Free
- Register: thriveumpqua.com
- Contact: connect@thriveumpqua.com
Printable version of this resource is available for distribution in clinical settings. To request PDF file, contact deverson@umpquahealth.com.
Network News
Network Changes: Additions/Termed
Termed Providers
The following providers have been removed from the Umpqua Health Alliance network:
| Provider Name | Facility | Effective Date |
| Alyssa Davidson, CSWA | Juniper Tree Counseling | 12/31/2025 |
| Holly Battleson, QMHP | Adapt Integrated Health | 12/31/2025 |
| Fatima Jalloh, LCSW | Adapt Integrated Health | 01/02/2026 |
| Genevieve Murstig, RD | PeaceHealth | 01/05/2026 |
| Brynn Roche, CRNA | PeaceHealth | 12/29/2025 |
| Chelesia Burkes-Brown, MSN | Cow Creek Health and Wellness | 01/09/2026 |
| Viseh Sundberg-Movarekhi, DDS | Advantage Dental | 11/22/2025 |
| Desiree Knechtges, RD | Mom’s Meals | 01/13/2026 |
| Rodney Deaton, MD | PeaceHealth | 01/05/2025 |
| Denise White, NP | PeaceHealth | 11/24/2025 |
| Genoa Ferguson, MD | Oregon Urology | 12/31/2025 |
| William Doubledee, LPC | Adapt Integrated Health | 01/28/2026 |
| Robert Brown, CADC | Adapt Integrated Health | 01/21/2026 |
| Alainnah Knight, LPC | Adapt Integrated Health | 01/26/2026 |
| Joan Harvey, NP | Oregon Urology | 12/31/2025 |
| Michael Smith-Fernandez, LCSW | Second Wind Mental Health | 01/15/2026 |
| Joshua Allen Miller, CADC | Adapt Integrated Health | 01/26/2026 |
| Deborah Ann Ramirez, QMHA | Adapt Integrated Health | 01/20/2026 |
| Eric Ory, MD | CEP America | 01/20/2026 |
| Julie Sparlin, DM | CEP America | 01/20/2026 |
| Kerry Kreidel, MD | CEP America | 01/20/2026 |
| Natalie Mackintosh, MD | CEP America | 01/20/2026 |
| Vanessa Vu, MD | CEP America | 01/20/2026 |
| Richard Veerman, MD | PeaceHealth | 01/22/2026 |
| Jennifer Hope, PMHNP-BC | Hope Mental Wellness | 01/30/2026 |
New Providers
The following providers have joined the Umpqua Health Alliance network:
| Provider Name | Facility | Effective Date |
| Alainnah Knight, LPC | Adapt Integrated Health | 09/24/2025 |
| Christine Crank, MD | PeaceHealth | 02/11/2025 |
| Jennifer Janowiecki, NP | PeaceHealth | 12/12/2025 |
| Jenifer Lingeman, MD | PeaceHealth | 12/12/2025 |
| John Alharsami, CADC-I | Adapt Integrated Health | 12/08/2025 |
| Rachel Brown, PSS-AA, PSS-AMH | Adapt Integrated Health | 12/08/2025 |
| Ivy Doolittle, CADC-I | Adapt Integrated Health | 04/08/2025 |
| LaFaye Grooms, QMHP-CERT | Adapt Integrated Health | 12/08/2025 |
| Tiffany Pagel, QMHA-R | Adapt Integrated Health | 12/03/2025 |
| Lan Gao, DDS | Advantage Dental | 11/03/2025 |
| Tiffany Chaille, NP | PeaceHealth | 01/06/2026 |
| Virginia Moore, NP | PeaceHealth | 12/01/2025 |
| Melissa Benson, PSS-Fs | Adapt Integrated Health | 09/24/2025 |
| Melony Coleman, QMHP-R | Adapt Integrated Health | 10/24/2025 |
| Cynthia Smith, QMHA-R | Adapt Integrated Health | 12/18/2025 |
| Tracey Walker, QMHP-R | Adapt Integrated Health | 01/09/2026 |
| Charles Anderson, MD | CEP America | 12/15/2025 |
| Jeffrey Poulsen, MD | CEP America | 10/27/2025 |
| Ngoc-Hai Truong, MD | CEP America | 12/22/2025 |
| Wai Lee, MD | CEP America | 12/22/2025 |
| Mary McKee, MD | PeaceHealth | 01/16/2026 |
Year-End Claims Submission Reminder
As the new reporting cycle begins, complete and timely claims submission is essential to ensure accurate 2025 rates and quality measure calculations. Providers and delegates are asked to review and submit all outstanding claims, including corrected or resubmitted claims, to support complete data capture for services delivered during the year.
To avoid processing delays, claims should be submitted as soon as possible, with a preferred completion date by the end of February 2026. The final deadline for submission is March 9, 2026.
Timely submission supports accurate reporting and helps prevent last-minute issues that may affect final results, including missing data, claim corrections or delayed processing. Early submission also allows additional time to resolve questions or address errors if needed. Providers who anticipate delays or need assistance with claims submission are encouraged to reach out promptly for support.
MTM Training Video Now Available
A new Medically Tailored Meals training video is now available on the Umpqua Health Alliance website. The video provides an overview of the Medically Tailored Meals benefit and outlines tools and resources to support clinics in identifying eligible members and facilitating access to services. It is intended for providers and care teams involved in screening, referral or care coordination related to nutrition and health-related social needs.
The training reviews eligibility considerations, referral pathways and key roles for clinical and nonclinical staff. It may be useful for onboarding new team members or as a refresher for staff supporting members with qualifying conditions.
Providers may also wish to reference the HRSN Medically Tailored Meals Benefit Overview for Clinics, which summarizes benefit details and clinical considerations in a printable format.
Detailed eligibility and workflow guidance is available in the Practice Tactics section.
- MTM Training Video:
https://www.umpquahealth.com/form/medically-tailored-meals/ - HRSN MTM Benefit Overview for Clinics (PDF):
https://www.umpquahealth.com/wp-content/uploads/2025/12/mtm-benefit-overview-for-clinics-en.pdf
On the Lookout
Recent Changes to Vaccine Schedules
The Centers for Disease Control (CDC) and the Advisory Committee on Immunization Practices (ACIP) that advises the CDC have made several recent changes to the childhood and adolescent immunization schedules. In December 2025, ACIP changed a several decade long recommendation of offering the Hepatitis B vaccine universally at birth to an “individual-based decision making for mothers of infants who test negative for hepatitis B.” In January 2026, The Secretary of the US Department of Health and Human Services (HHS) and the CDC changed the childhood and adolescent vaccination schedule.
The CDC updated their online vaccine schedule to remove the recommendation for vaccines for the following diseases from routine recommended to now only recommended for high-risk individuals: rotavirus, hepatitis A, hepatitis B, meningococcal, RSV, flu/influenza. These are now recommended for “high-risk groups or populations” or labeled as immunizations based on “shared clinical decision making.” The following diseases were kept on the recommended routine vaccine schedule: measles, mumps, rubella, pertussis, tetanus, diphtheria, HiB, pneumonia, polio, chickenpox/varicella and HPV.
These changes were not based on any new scientific evidence or epidemiological data nor did they follow the established ACIP process of scrutiny and review.
The childhood and adolescent vaccine schedules have often been complex and confusing for many parents and this change has already seeded more confusion and doubt in the utility and safety of vaccines to prevent morbidity and mortality.
In response, the Oregon Health Authority (OHA), Western Coast Health Alliance and the American Academy of Pediatrics (AAP) have all stated (among many other health organizations) that they are still practicing and recommending the old childhood and adolescent schedule (prior to January 5th, 2026). As of writing this, the CCO metrics related to childhood and adolescent immunizations have not changed.
Conversations about vaccines and vaccine preventable diseases are already increasing in the clinical setting as a consequence of these changes. If you would like copies of the schedule being followed by OHA and AAP please contact DPHN. If you would like patient facing materials to encourage dialogue with patients or would like training on evidence based modalities (such as motivational interviewing) on how to talk with patients about this change please contact DPHN.
Dental Digest
Can Oral Health Be Inherited?
Oral health is influenced by a combination of genetics, environment and daily habits. While conditions such as tooth decay and gum disease are not inherited directly, genetic factors can affect traits like enamel strength, tooth structure and susceptibility to certain oral health issues.
A recent article from Advantage Dental explores how inherited factors may contribute to oral health risks and highlights the role of preventive care in reducing those risks. The article also emphasizes the importance of regular dental visits, good oral hygiene practices and early intervention, particularly for children and families with a history of dental issues.
This resource may be helpful for providers when discussing oral health risk factors with members and reinforcing the value of preventive dental care.

