Provider Newsletter September 2018
 Practice Tactics
Practice Tactics
October Prioritized List Updates
The Prioritized List has been updated for October 1, 2018. The proposed list can be accessed here, and a complete discussion of the changes are discussed in detail here.
Notable changes include:
- Multiple additions/pairings to CV condition lines
- Expanding use of neuropsychological testing to several conditions (PTSD, TBI, dementia)
- Further narrowing definitions of covered Acne
- Adding Home Light Therapy to treatment of severe inflammatory skin disease (psoriasis, atopic dermatitis, etc.)
Guideline Note changes:
- Urine drug testing in the setting of SUD and chronic opioid prescribing
- Obstructive Sleep Apnea: Home Sleep Studies preferred (already adopted)
- PTSD
- Implantable Cardiac Defibrillators
- Deep brain stimulation for Parkinson’s Disease
- Cancer: narrowing PET use, palliative radiotherapy to bones
New Addition to Umpqua Health Alliance Team
UHA is excited to announce the addition of our new Quality Director, Tanveer Bokhari, MBBS. He performed a similar role with Family Care. Tanveer has been meeting with provider groups, and has already released a provider-friendly tool for use with the CCO Quality metrics.
This tool is a new feature for the Provider Portal. This new feature will allow users to address gaps in real time and remove members from “Gap Opportunities” for a set period of time – click here to view a user guide with step by step instructions to assist you in navigating the new feature. If you do have any questions or need additional assistance please feel free to contact Tanveer.
Standard vs Expedited Prior Authorizations
UHA processes prior authorizations according to regulations. The standard time frame for a decision is 14 calendar days. An expedited decision can be requested if the standard review time would seriously jeopardize the patient’s life or health or ability to attain, maintain, or regain maximum function. Expedited requests for Prior Authorizations should be reserved for truly emergent conditions (think STAT).
It may be in the patient’s best interest to have the request processed within the standard time frame so that UHA has time to follow up if clarification is needed or to obtain supporting documentation that could improve the likelihood of a favorable determination. The expedited time frame of 72 hours may limit the opportunity to obtain necessary information, especially if impacted by offices that are closed over the weekend.
If a request must be expedited, providers must ensure that the information submitted clearly demonstrates medical necessity for the time frame and contains all necessary information for review.
A reminder: PA’s are not required for In-Network providers (except Dermatology); it is best to send the PA at the same time that you are making the appointment with the consultant.
CIM Users
UHA transitioned to PH Tech’s Community Integration Manager (CIM) effective January 1, 2018 and many of our provider’s offices have obtained access to the portal for entering prior authorizations. CIM users have agreed to not disclose, or permit anyone other than themselves, to use their information to access the system.
We want to remind our providers and their office staff that each individual user has their own unique username and password that should not be shared with any other individuals, even if multiple users are within the same office. Users should ensure their information is current and that they notify PH Tech of any new, updated, or terminated access.
Unauthorized use will be reported to PH Tech’s compliance department and the user’s access will be terminated.
If you need to update your CIM user information, request new access, or terminate access, please contact PH Tech’s technical support at 503-584-2169, option #2.
 Umpqua Health – Newton Creek Update
Umpqua Health – Newton Creek Update
You can’t miss the beautiful new building on NE Stephens Street. The nearly 25,000 square foot clinic is a sight to behold, with its modern metal exterior and two-story wall of windows. As our construction crews are putting the finishing touches on Umpqua Health – Newton Creek, we are working to map out clinic operations.
The new clinic will feature an urgent care, pediatrics, primary care and behavioral health. With all of these moving pieces, Umpqua Health is establishing a Provider Operating Council (POC). The council, which will consist of six providers and three Umpqua Health management staff members, will help to guide strategy and processes at both UH – NC and its exiting clinic location, UH – Harvard.
Umpqua Health is also excited to announce that Dr. Layne Jorgensen, DO will be joining the Umpqua Health team at the Newton Creek clinic. Dr. Jorgensen has been a leader in health care in Douglas County for years, and Umpqua Health is proud to have him joining our care team. In addition to continuing to be a practicing physician, Dr. Jorgensen will also be the provider leader of the Umpqua Health Clinics group as its Chief Clinical Officer.
Construction at Umpqua Health – Newton Creek is on schedule, and providers will start seeing patients at the new facility in early December.
 On the Lookout
On the Lookout
With the new school year starting, it’s an excellent time for parents to consider making sure their children’s required immunizations are up to date. Oregon law requires all children (who have not provided valid documentation of a medical or non-medical exemption) to be up to date on required immunizations in order to attend school.
Every year Douglas Public Health Network conducts a review of schools’ student immunization reports countywide. If a student is not up to date on their immunizations with no valid exemption, an Exclusion Letter will be sent to both the school and the student’s parents. This letter will provide notification of the deadline by which the child’s immunizations must be up to date in order for them to attend school. Once valid exemption documentation or documentation that immunizations are up to date has been provided to the school, the student will be able to return. The exclusion date deadline for the coming school year is February 20, 2019.
To protect their children and those around them, and to avoid the hassle of having to obtain immunizations at the last minute or face exclusion, parents should verify their children’s immunization status with their child’s provider. Providers with school-age children in their practices should remind parents about these requirements and encourage them to get their children up to date. We also encourage parents to discuss with providers any additional vaccines that may be available for their child, which can provide additional protection for their children’s health, such as the HPV or meningococcal vaccines. The meningococcal vaccines are especially important for college-age students going to universities in Oregon.
Immunizations required for Kindergarten through 12th Grade
| DTaP | Polio | Varicella | MMR | Hepatitis B | Hepatitis A | Hib | Tdap | |
| K or Grades 1 – 6 | 5 | 4 | 1 | 2 | 3 | 2 | ||
| Grades 7 – 9 | 5 | 4 | 1 | 2 | 3 | 2 | 1 | |
| Grades 10 – 12 | 5 | 4 | 1 | 2 | 3 | 1 |
 Medical Management
Medical Management
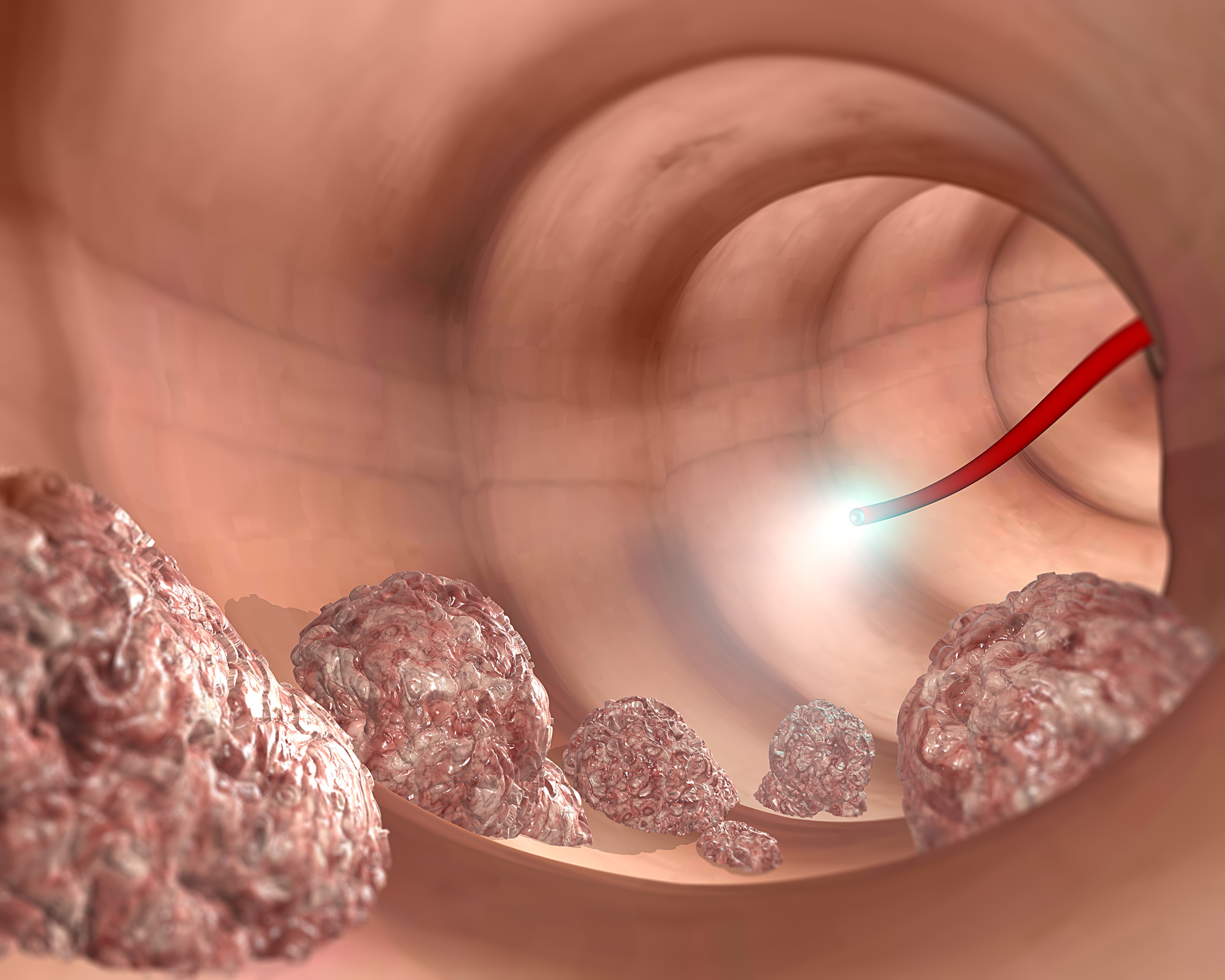
The Use of Colonoscopy as a Screening Tool for Colo-rectal Cancer: Defining Medical Necessity
Colonoscopy is the most accurate exam used to detect and prevent cancer of the colon and rectum. It can find cancer early and save lives. But even a very good exam can be done too often. When therefore is it indicated and when is it not?
Colorectal Cancer (CRC) is the second leading cause of cancer-related death in the United States. Colonoscopy plays a central role in the CRC screening process and can be performed for several indications ranging from screening to surveillance to a diagnostic work-up for a broad range of clinical conditions. In the setting of guaiac positive stool, change in bowel habits, alterations in stool caliber, recurrent abdominal pain, colonoscopy has replaced most other diagnostic studies such as barium enema, CT scans and CT colonography. In the case of the above-mentioned symptomatology, the use of a diagnostic colonoscopy is strongly supported in the literature. However, in the absence of a moderate to high suspicion of CRC, inappropriate screening is not warranted.
The American Gastroenterology Association and the American College of Surgeons have supported the Choosing Wisely approaches to diagnostic screening. These organizations support the avoidance of colorectal cancer screening tests in asymptomatic patients with a life expectancy of less than 10 years and no family or personal history of colorectal neoplasia.
Screening for colorectal cancer has been shown to reduce the mortality associated with this common disease; colonoscopy provides the opportunity to detect and remove adenomatous polyps, the precursor lesion to many cancers, thereby reducing the incidence of the disease later in life.
However, screening and surveillance modalities are inappropriate when the risks exceed the benefit.
The risk of colonoscopy increases with increasing age and comorbidities.
The risk/benefit ratio of colorectal cancer screening or surveillance for any patient should be individualized based on the results of previous screening examinations, family history, predicted risk of the intervention, life expectancy and patient preference.
Having a colonoscopy more than once every five or ten years usually isn’t necessary
A polyp, in the colon or rectum is common in adults and usually harmless. But some polyps—known as adenomas—may eventually turn into cancer. Doctors can spot and remove polyps during a colonoscopy. If the test doesn’t find adenomas or cancer and one does not have risk factors for the disease, the chance of developing it is low for the next 10 years. That’s because the test misses very few adenomas, and colorectal cancer grows slowly. Even if one or two small, low-risk adenomas are removed, a patient is unlikely to develop cancer for at least five years, and repeating the test sooner provides little benefit. Most individuals need the exam just once a decade, and only a few with larger, more serious polyps may need it more often than every five years.
Risks Associated with Colonoscopy
Colonoscopy is a safe procedure. Occasionally it can cause heavy bleeding, tears in the colon, inflammation or infection of pouches in the colon (diverticulitis), severe abdominal pain, and problems in people with heart or blood vessel disease. Some complications can lead to blood transfusions, surgery, hospitalization, or rarely, death. The test also has inconveniences. Patients must restrict their diet and take laxatives beforehand.
It can be expensive
A colonoscopy typically costs about $1,100 and with polyp removal, about $1,500, according to healthcarebluebook.com. With the advent of the Affordable Care Act, screening procedures defined as medically necessary by the United States Preventive Task Force must be covered  in full by all health plans. While Medicare and many health plans cover the exam, they may not if the exam is performed more often than necessary. Patients may also be responsible for charges related to polyp removal and anesthesia. Anesthesia using Diprivan (Propofol) generally is not recommended or deemed medically necessary by many health plans for routine, screening colonoscopies.
in full by all health plans. While Medicare and many health plans cover the exam, they may not if the exam is performed more often than necessary. Patients may also be responsible for charges related to polyp removal and anesthesia. Anesthesia using Diprivan (Propofol) generally is not recommended or deemed medically necessary by many health plans for routine, screening colonoscopies.
Colon cancer screening should begin at age 50 for most people. Patients with a family history of colorectal may be advised to begin screening earlier than age 50. If a colonoscopy doesn’t find adenomas or cancer, patients without risk factors should not have a repeat exam within 10 years. If one or two small, low-risk adenomas are removed, the exam should be repeated in five to 10 years.
In the presence of a comorbidity such as inflammatory bowel disease or Crohn’s Disease, screening intervals may be shortened due to severity of symptoms. In the setting of a history of multiple, large, or high-risk adenomas more frequent screening may be recommended. Routine checks usually aren’t needed after age 75 from a cost-benefit analysis.
Quality Metrics and Colonoscopy
Accurate determination of indication for colonoscopy is critical for several quality metrics. For example, the Adenoma Reduction Rate (ADR) – defined for each colonoscopist by the percent of patients with at least one adenoma among those undergoing screening colonoscopy – has become an important metric for measuring colonoscopy quality. Given the consistent observed inverse relationship between ADR and interval cancers, the Centers for Medicare And Medicaid Services (CMS) included ADR in its list of 2014 Physician Quality Reporting System (PQRS) measures and the American College of Gastroenterology (ACG) published target ADRs for average-risk screening exams. However, ADRs could be falsely elevated if surveillance or diagnostic colonoscopies are misclassified as screening exams given the prevalence of adenomas differs by exam indication. Therefore, accurate determination of the indication for colonoscopy is necessary to accurately assess ADRs and compare the performance of a colonoscopist to his/her peers and national benchmarks.
Accurate characterization of colonoscopy under- and overuse is also dependent on careful assessment of colonoscopy indication. Quality and research work addressing under- and overuse has potential to improve the value of colonoscopy by improving outcomes (through addressing underuse) and reducing risk (through addressing overuse). Accordingly, CMS has designated recommendations for the appropriate timing of repeat colonoscopy after normal average-risk screening as a PQRS measure. Additionally, the American Gastroenterological Association (AGA) has partnered with the American Board of Internal Medicine (ABIM) Foundation as part of the “Choosing Wisely” campaign to promote appropriate screening and surveillance intervals after colonoscopy. However, appropriate intervals are based on several factors, including exam indication and findings at the time of prior colonoscopy. For example, guidelines recommend a 10-year interval for repeat colonoscopy in an average-risk patient with a normal screening exam; however, a five-year interval would be appropriate in a patient undergoing surveillance for a personal history of adenomatous polyps. Similarly, a repeat colonoscopy for surveillance two years after a colonoscopy with a small tubular adenoma, without high-grade dysplasia, would be considered overuse, whereas a diagnostic colonoscopy for gastrointestinal (GI) bleeding at that same time interval would be appropriate. Thus, without careful adjudication of indication, assessment of colonoscopy under- and overuse is impossible.
Finally, accurate determination of indication is also important for comparative effectiveness research of different CRC screening tests and strategies. When evaluating the effectiveness of screening tests to reduce interval cancers and mortality, it is important to exclude exams done for non-screening purposes, particularly diagnostic exams. A recent case-control study demonstrated an association between screening colonoscopy and reduced rates of right- and left-sided late-stage CRC; however, the authors found this association was stronger in colonoscopies done for screening purposes (OR 0.30, 95%CI 0.15–0.59) than those done for surveillance (OR 0.38, 95% CI 0.15–1.0), or “probable diagnostic” intent (OR 0.48, 95% CI 0.18–1.24). Overall, from clinical, healthcare quality, and clinical research perspectives, accurate assessment of indication for colonoscopy is vital.
 CME For Thee
CME For Thee
Umpqua Health Alliance strives to help providers identify opportunities to learn about new and developing areas in medicine. As part of that, UHA will occasionally share continuing medical education (CME) opportunities. If you come across an event offering CME that you’d like to share, please contact Kat Cooper.
For more information on the upcoming Tri-County Conference on Older Adult Issues, click here.